Osteoarthritis on Hip: Top Strategies for Managing Pain and Improving Mobility
Hip osteoarthritis, also known as osteoarthritis on hip, is a degenerative joint condition that can cause pain, stiffness, and limited mobility, significantly impacting an individual’s quality of life. Understanding the condition and learning how to manage its symptoms through a combination of treatment options, lifestyle adjustments, and home remedies is essential for maintaining overall joint health and reducing the impact of osteoarthritis on hip in daily life.
Key Takeaways
-
Understand the anatomy of the hip joint and how osteoarthritis develops in order to effectively manage symptoms.
-
Diagnose accurately with imaging, lab tests, physical assessments, and personalized treatment plans created with healthcare professionals.
-
Utilize lifestyle adjustments such as diet management & gentle exercise. Consider advanced therapies for pain relief & improved functional outcomes.
Understanding Hip Osteoarthritis
Hip osteoarthritis is a form of degenerative joint pain caused by the breakdown of the joint’s cartilage over time, which can lead to inflammation, stiffness, and pain. Comprehending the anatomy of the hip joint, osteoarthritis development in the hip, and associated symptoms is instrumental in effectively managing hip pain and maintaining joint health.
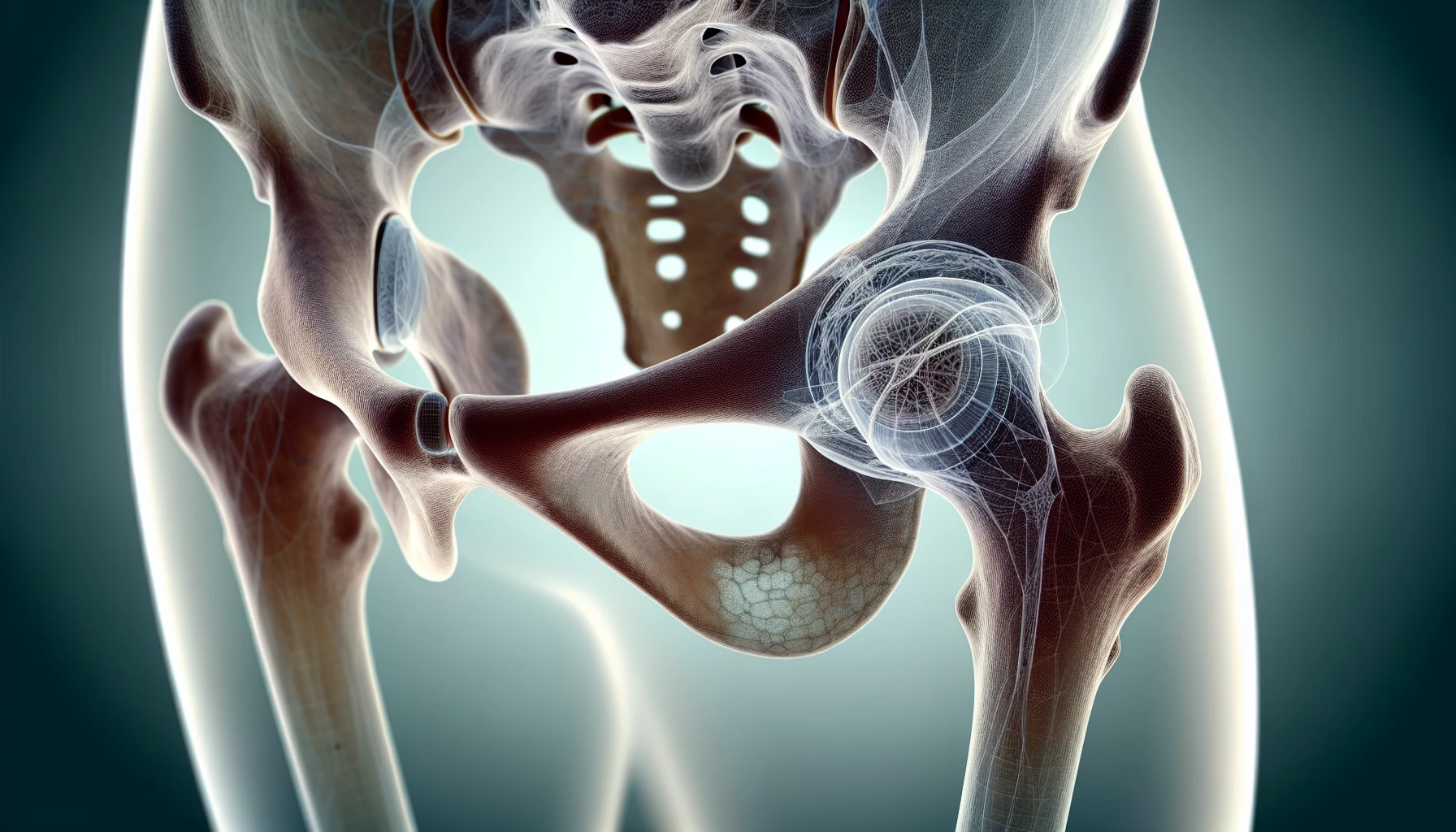
The Anatomy of the Hip Joint
The hip joint is a ball-and-socket joint that connects the femur to the pelvis, playing a vital role in mobility and stability. The head of the femur forms the ball, while the acetabulum forms the socket. The joint is stabilized by ligaments, muscles, and tendons, and is enveloped by a capsule filled with synovial fluid. Comprehending the hip and knee joints’ structure, including the knee joint, is instrumental in understanding the relationship between hip and knee pain.
Conditions such as femoroacetabular impingement (FAI), cam and pincer lesions, and torn acetabular labrum can affect the hip joint and contribute to knee and hip pain. These conditions can restrict the normal range of motion of the ball and socket joint and damage the cartilage, leading to further hip problems, knee injuries, and the potential onset of hip osteoarthritis. In some cases, individuals may also experience knee pain cold sensations due to the inflammation and restricted blood flow in the affected area.
How Osteoarthritis Develops in the Hip
Hip osteoarthritis develops as the cartilage within the joint breaks down over time, leading to changes in the underlying bone that can deteriorate and cause impaired function or disability. The hips and knees are particularly vulnerable to osteoarthritis due to their weight-bearing role. In the early stages of osteoarthritis, the cartilage between the joints is subject to wear and tear, as well as inflammation, which leads to the loss of water in the joint. This causes the cartilage to harden, making the surrounding joint more rigid and leading to bone-to-bone rubbing.
Avascular necrosis is another condition that can contribute to osteoarthritis pain and occurs when the blood supply to the ball at the end of the thigh bone is compromised. Identifying the progression of hip osteoarthritis aids in determining suitable treatment options and enhancing joint health.
Common Symptoms of Hip Osteoarthritis

Typical signs of hip osteoarthritis include pain, swelling, stiffness, and restricted range of motion. The initial indicators of osteoarthritis may include pain in the groin region, stiffness in the hip joint, and difficulty moving the joint. As the condition progresses, pain may worsen, and individuals may experience abnormal sensations in the hip joint and surrounding area.
It is also important to be aware of trochanteric bursitis, an inflammatory condition that may present as swelling, heat, and pain in the hip area. This condition can become chronic, and its treatment typically involves rest, analgesics, and physical therapy.
Identifying the symptoms of hip osteoarthritis is fundamental for seeking suitable treatment and effectively managing the condition.
Diagnosing Hip Osteoarthritis

Accurate diagnosis of hip osteoarthritis is key to determining suitable treatment options and managing the condition effectively. The diagnostic process involves:
-
A physical examination
-
Imaging tests such as X-rays
-
Laboratory tests to assess the severity of the osteoarthritis and rule out other potential causes of hip pain.
What to Expect During Your Doctor’s Visit
When visiting the doctor to discuss hip pain and the potential diagnosis of osteoarthritis, it is important to be prepared to answer questions about your hip pain, such as when it started, its location, and whether anything worsens or alleviates the pain. The doctor may also inquire about any recent injuries or trauma, previous hip surgeries or conditions, and any activities or movements that aggravate the pain.
During the physical examination, the doctor will assess for posterior hip pain during squatting, pain on abduction or adduction, and evaluate for adductor weakness. These assessments will help the doctor determine the presence of hip osteoarthritis and recommend further diagnostic tests if necessary.
Imaging and Lab Tests for Accurate Diagnosis
Imaging tests such as X-rays, MRIs, and arthrogram investigations are utilized to diagnose hip osteoarthritis and provide a detailed image of the bones, soft tissues, and cartilage in the hip joint. X-rays can reveal signs of wear and damage in the hip joints and pelvic bones, demonstrating the degree of arthritis and supplying radiographic proof of osteoarthritis in the hip joints.
Laboratory tests may also be employed to confirm the diagnosis of hip osteoarthritis and rule out other potential causes of hip pain. By combining physical examinations, imaging tests, and laboratory tests, physicians can provide an accurate diagnosis and recommend appropriate treatment options.
Treatment Options for Hip Osteoarthritis

There are a variety of treatment options available for hip osteoarthritis, including first treatments, non-surgical treatments, and surgical alternatives. The choice of treatment depends on the severity of the condition and the individual’s preferences and lifestyle.
It’s important to consider all possible treatment options and collaborate with healthcare professionals to devise a personalized treatment plan.
First Treatments, Full Spectrum CBD and other supplements
Initial treatment options for hip osteoarthritis include the use of over-the-counter pain relievers, such as non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen, to manage pain. Full Spectrum CBD has also been studied for its potential in treating pain and inflammation associated with hip osteoarthritis, but further research is necessary to accurately assess its efficacy.
Other supplements that may be beneficial for hip osteoarthritis treatment include:
-
Glucosamine
-
Chondroitin
-
Curcumin
-
Green tea
-
Vitamin D
-
Omega-3 fatty acids
These supplements may help protect and repair cartilage, reduce inflammation, and alleviate joint pain, making them a valuable addition to the first-line treatment of hip osteoarthritis.
Non-Surgical Treatments
Non-surgical treatments for hip osteoarthritis include:
-
Activity modification
-
Exercise prescription and strength training
-
Physiotherapy modalities such as manual therapy
-
Medication (including over-the-counter non-steroidal anti-inflammatory drugs)
-
Corticosteroids for immediate pain relief
Physical therapy, in particular, can help enhance strength, range of motion, and mobility while managing pain and restoring normal movement in the hip and legs.
Injections, such as cortisone or hyaluronic acid, can also be utilized to alleviate the symptoms of hip osteoarthritis by decreasing inflammation in the joints and providing rapid pain relief. The effects of these injections can last from several weeks to several months, making them a valuable non-surgical treatment option for those with hip osteoarthritis.
Surgical Alternatives: When Is Hip Replacement Surgery Needed?
Hip replacement surgery may be considered for those with severe hip osteoarthritis when all other conservative measures have been exhausted. There are several types of hip replacement surgeries available for osteoarthritis, including:
-
Total hip replacement
-
Partial hip replacement
-
Hip revision surgery
-
Hip arthroplasty
-
Hip resurfacing
The choice of surgical alternative depends on the severity of the hip osteoarthritis, the patient’s overall health, and their personal preferences.
Hip pain relief is a common goal for those considering joint replacement surgery, and hip replacement surgery, in particular, has a high success rate. Approximately 95% of patients report significant improvement after the procedure. However, before opting for this treatment, potential risks and complications need to be taken into account. These include:
-
Blood clots
-
Infection
-
Nerve damage
-
Dislocation risk
-
Residual aches
It is important to discuss these risks with your doctor and weigh them against the potential benefits of the surgery.
Lifestyle Adjustments and Home Remedies
Making lifestyle adjustments and utilizing home remedies can help manage hip osteoarthritis symptoms and improve overall joint health. Incorporating a healthy diet, engaging in gentle exercise, and managing stress can all contribute to reducing pain, increasing mobility, and maintaining a normal active lifestyle.
The Role of Diet and Weight Management
Adhering to a healthy diet and maintaining a balanced weight is key for controlling hip osteoarthritis symptoms and preventing additional joint damage. Weight management has a considerable influence on the progression of hip osteoarthritis, as obese individuals are more susceptible to faster and more severe disease progression. Research indicates that weight loss can reduce pain and yield better results in hip osteoarthritis.
A well-balanced diet for patients with hip osteoarthritis should incorporate anti-inflammatory foods such as fruits, vegetables, lean protein, and omega-3 fatty acids. Consuming oily fish like salmon and mackerel, which are rich in omega-3 fatty acids and possess natural anti-inflammatory properties, is highly recommended. Additionally, it is advised to abstain from foods high in total and saturated fat.
Incorporating Gentle Exercise Into Your Routine

Engaging in gentle exercise can help alleviate joint discomfort, increase mobility, and boost blood circulation for those with hip osteoarthritis. Some recommended exercises for hip osteoarthritis include mini squats, hip stretches, and gentle hip exercises. To safely incorporate gentle exercises into your daily routine, start with low-intensity exercises and gradually increase the intensity, avoiding high-impact aerobic exercises such as running and jumping rope.
Using exercise equipment like recumbent bikes or ellipticals can also be beneficial for individuals with hip osteoarthritis, as they provide low-impact exercise options that can help improve mobility and manage pain. Always consult a doctor or physical therapist before starting a new exercise regimen to ensure the exercises are appropriate for your specific condition.
Stress Management and Its Impact on Joint Health
Stress can exacerbate symptoms of hip osteoarthritis, leading to increased joint pain and inflammation, fatigue, disability, and a depressed mood. Effectively managing stress can significantly improve overall well-being for those with hip osteoarthritis. Here are some techniques to consider:
-
Massages
-
Mindfulness and meditation exercises
-
Exploring alternative therapies
-
Participating in self-management programs
-
Engaging in physical activity
By practicing stress management techniques, hip osteoarthritis patients may experience reduced stress levels, improved relaxation, and enhanced mental and emotional health. This can lead to better pain management, improved sleep, improved mood, and an increased overall quality of life.
Advanced Therapies and Research
Recent developments in hip osteoarthritis treatment include:
-
Injectables for joint repair and pain relief
-
Potential new treatments with disease-modifying and analgesic properties
-
Injectable cell therapy
-
Hip arthroplasty, a form of joint replacement
Research on regenerative medicine, such as stem cell therapy, has shown potential in providing pain relief and functional improvement for individuals with hip osteoarthritis by addressing the issue of destroy joint tissue. However, further research is needed to accurately determine the full efficacy of these advanced therapies for hip osteoarthritis.
As research and technology persistently evolve, staying updated about the latest developments and potential treatment options for hip osteoarthritis is key. These cutting-edge therapies may provide new hope and improved outcomes for those living with this debilitating condition.
Summary
Hip osteoarthritis is a complex condition that requires a comprehensive understanding of its causes, symptoms, and treatment options. By learning about the anatomy of the hip joint, the development of osteoarthritis, and the wide array of treatment options available, individuals with hip osteoarthritis can effectively manage their symptoms and maintain a normal active lifestyle. Embracing lifestyle adjustments, such as maintaining a healthy diet, engaging in gentle exercise, and managing stress, can significantly improve overall joint health and quality of life. Stay informed about the latest advancements in treatment and research, and work closely with healthcare professionals to develop a personalized treatment plan that best addresses your unique needs and goals.
Frequently Asked Questions
Is walking good for hip osteoarthritis?
Walking is an effective form of exercise for people with hip osteoarthritis. It's low-impact, helps keep joints flexible, and helps to improve bone health. Gradually increase your speed and distance as you start a walking program; if you experience pain or stiffness, reduce the intensity and talk to your doctor.
What not to do with hip osteoarthritis?
Avoid high-impact exercises and activities that aggravate hip arthritis, and modify your lifestyle through weight loss for added stress relief. Incorporating physical therapy exercises can also help strengthen the hip joint.
What does osteoarthritis of the hip feel like?
Osteoarthritis of the hip is characterized by groin pain, stiffness and difficulty in movement. Additionally, the pain can be worsened after standing or walking for long periods of time, or even after a period of rest.
What age do people get osteoarthritis in their hips?
Osteoarthritis is more commonly seen in people over the age of 45, with women more likely to be affected than men. Symptoms typically appear in people over 50, but can also affect younger people and athletes.
What causes hip pain and knee pain at the same time?
Osteoarthritis is a common condition that can cause simultaneous hip and knee pain due to the gradual wearing down of cartilage in the joints.
